Developed as a fully integrated system, this software offers a wealth of features such as:-
- The Scheduling and Management of Appointments
- The direct entry by Doctors of their Claimant Medical Assessments
- Instant access to up-to-the-minute information tailored to each user’s needs
- The generation of flexible, automated Reports
- The automatic production of Bills
- The facilitation of BAU Operations for Medical Clinics.

An Independent Medical Examination (IME) is a medical evaluation performed by a medical professional on a patient who was not previously involved in the treatment of that patient, to evaluate the patient’s course of prior treatment and current condition. IMEs are conducted by doctors, psychologists, and other licensed
healthcare professionals in essentially all medical disciplines, depending on the purpose of the exam and the claimed injuries.
Such examinations are generally conducted in the context of a legal or administrative proceeding, at the request of the party opposing the patient’s request for benefits. IMEs are commonly held in the context of workers’ compensation cases, disability claims, and personal injury litigation.
The purpose of an IME is to provide an independent and objective assessment of the patient’s medical condition, which can be used to determine the extent of the patient’s injuries and the appropriate level of compensation
Examination and Management of IME’s Requests was an issue faced by multiple Insurance Company Vendors due to the high volume of manual paperwork involved, appointment scheduling and coordination, multiple doctors and various other inputs required.
It was realised that software could help with the efficient management of Claimant Personal Information, HealthCare Data, and Generating Customized Reports as per Insurance Companies standard.
- The vInnovate IMEZ Solution was developed as an integrated system, to conduct Independent Medical Examination through efficient Management of Claimant Personal Information, Healthcare Data, Appointment Scheduling and Summary Reports for Insurance Company Vendors.
- It also provides additional functionality for Claimant and Doctor Inputs with Flexible form Designs and Presets for Quick form filling
- It is scalable to perform operations across multiple Locations and Doctors with Separate login for Administrator and Receptionist
- It offers additional Support for Worker’s Compensation Examination
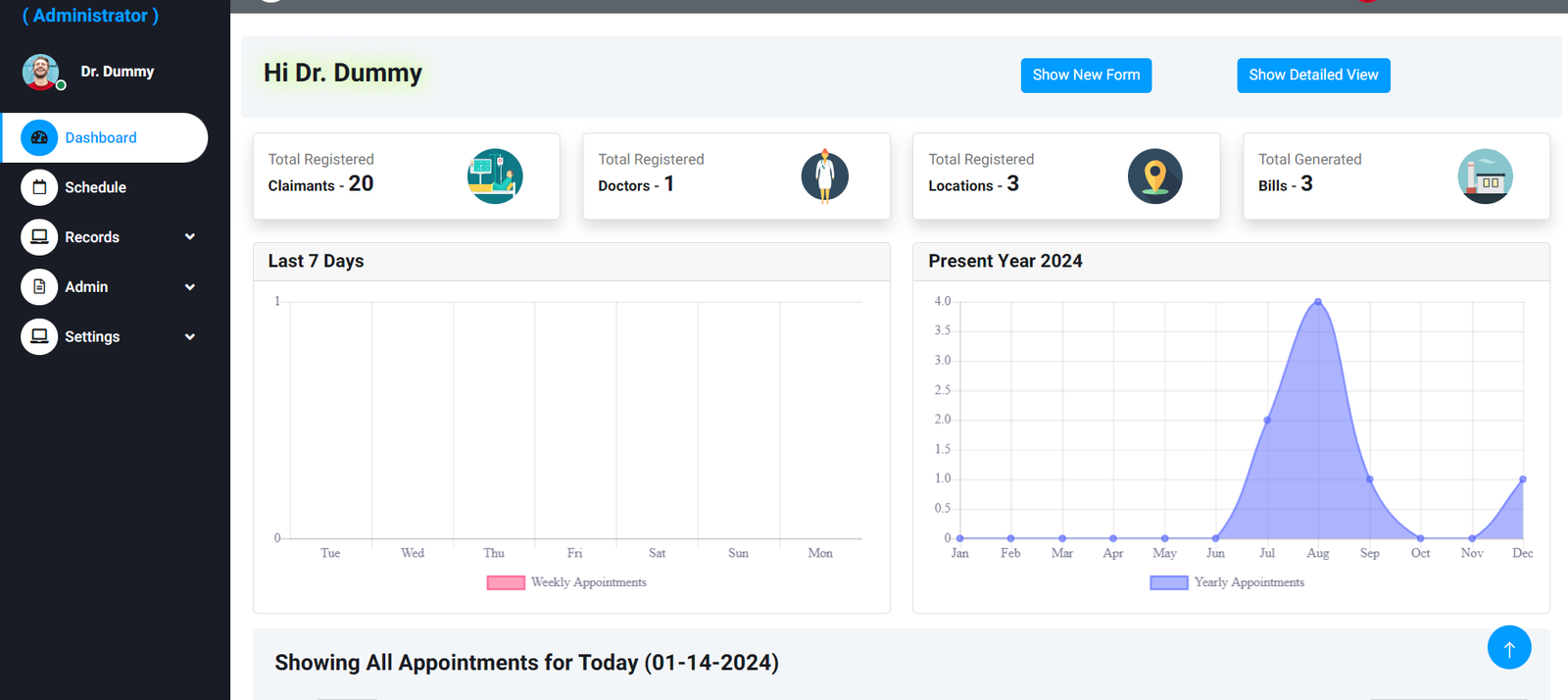
- All of above with Special Privileges for Administrator to monitor BAU process with personalized Dashboard, System Logs and Dedicated Appointment Management Screens
Features
This ‘feature-rich’ application provides:
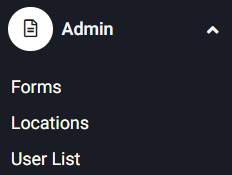
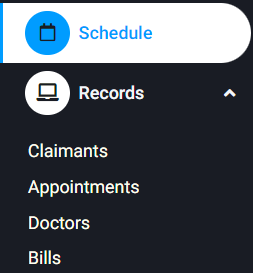
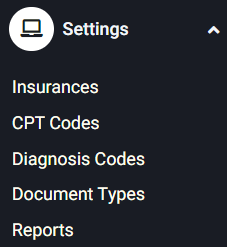
- Multiple actor login - Users(Receptionist) , Administrator; with fine-grained access control to allow each user to quickly access the information and functions he/she needs.
- Multiple actor login - Users(Receptionist) , Administrator; with fine-grained access control to allow each user to quickly access the information and functions he/she needs● A customisable user Dashboard to constantly display vital information, with ‘drill-down’ one click access to view more detail, and to update information.
- User-definable coding systems which enable individual organisations to use their preferred terminology and acronyms
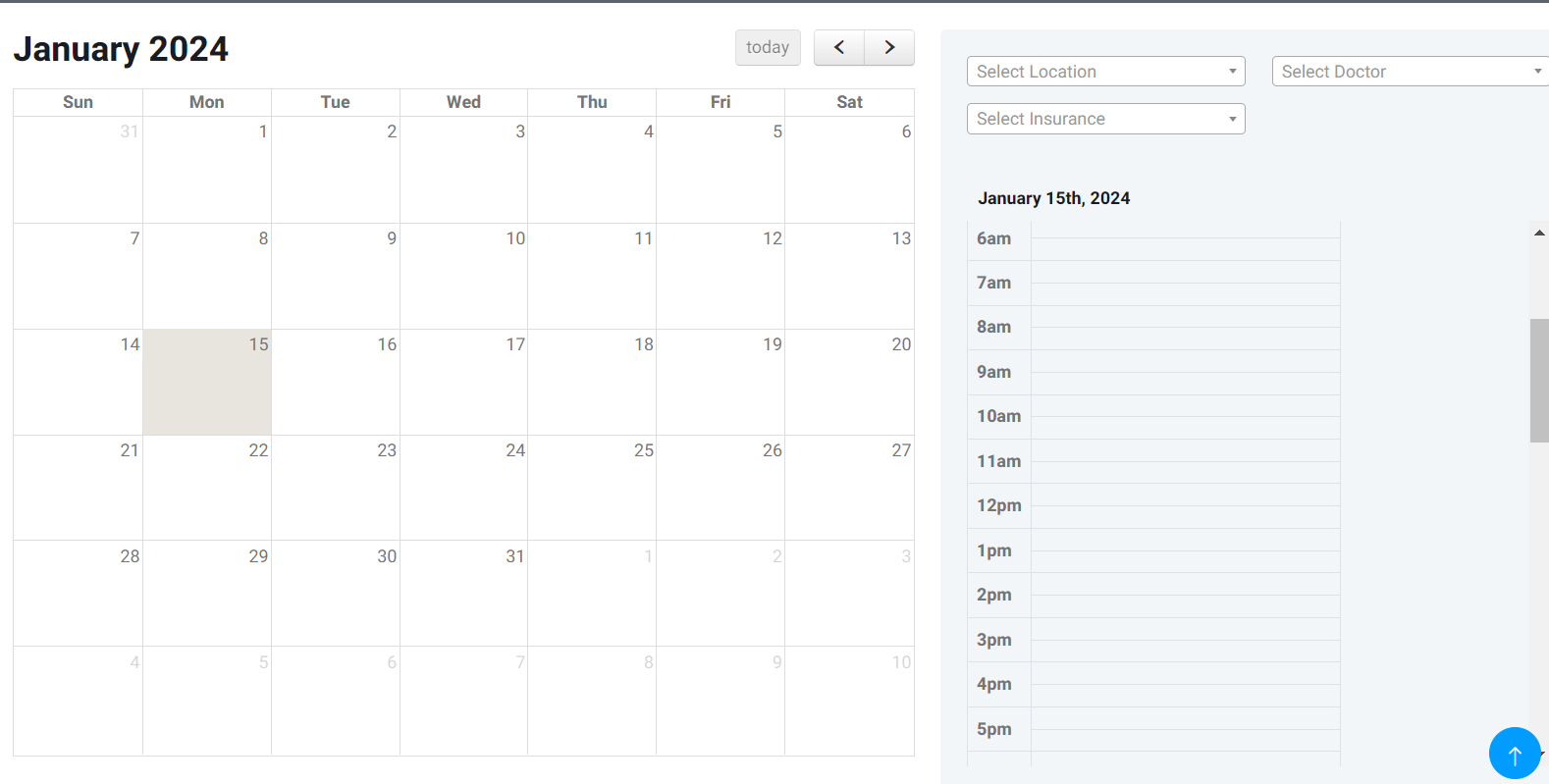
- Appointment scheduling for claimants with doctors provides a single, shared calendar to avoid errors and omissions
- A flexible forms design system with electronic distribution and management to ensure that everyone in the organisation receives information they need at the time they need it
- Auto-checking of claimant responses. This ensures that all responses received are logged and automatically checked for completeness, accuracy and required support documentation, before being stored in the appropriate location
- Dynamic Report Generation based on Claimant and Doctor response. Different responses often require different reporting and follow-up actions. The system recognises this and automatically creates the documentation in the appropriate format for the required actors
- A comprehensive Installation, training and support package ensures that your system gets off to a flying start and is set up and configured in the most efficient and productive way with your staff confident in its use.
- Digitization of the whole IME process allows all data to be efficiently stored and managed with confidentiality
- The enhanced ‘User Experience’ and also efficiency is achieved
- The efficiencies provided by the system results in more patients being handled without increasing the human resources deployed
- Historical saving of records in digital format allows for easy and quick access with powerful search functionality to locate specific pieces of information
WorkFlow
As with all aspects of the system, the workflow process is flexible and configurable to meet the needs of different situations. However, a typical process might include:-
- Administrator sets up users with access privileges
- Administrator creates forms and report templates,etc.
- System receives enquiries from claimants, which gets converted to appointment and triggers the issue of electronic messages and online forms
- Claimant submits completed electronic forms and required documents, which are automatically checked by the system for accuracy and completeness
- Doctor reviews claimant record and carries out necessary medical checks and tests
- Summary report gets generated.
Benefits
- Secure system design ensures that claimant confidentiality is maintained
- Flexibility and customisability ensure that the process fits each situation
- Full integration means that information is entered only once
- Automated routines for response checking and report generation mean that errors and omissions are minimised, and fraudulent claims are more easily identified
- Ongoing support ensures that your system is always fully optimised, and your staff are confident in its use